What Is Sleep Testing and Why Is It Done?
Sleep testing is a diagnostic procedure that monitors your body’s functions during sleep to identify sleep disorders. HealPolysomnography is considered the gold standard in sleep testing Sydney. This comprehensive overnight assessment records multiple body systems at the same time, including brain activity, heart rhythm, breathing patterns, muscle movements, and blood oxygen levels. The detailed data creates a complete picture of your sleep architecture and uncovers abnormalities that may not be detected through routine examinations.
Through sleep testing Sydney, clinicians can diagnose a wide range of sleep disorders, including:
- Obstructive sleep apnea: Repeated breathing interruptions caused by airway blockage
- Narcolepsy: Excessive daytime sleepiness and sudden sleep attacks
- REM sleep behavior disorder: Physical movement and actions during dreaming
- Periodic limb movement disorder: Repetitive arm or leg movements throughout sleep
- Insomnia: Ongoing difficulty falling asleep or staying asleep
Identifying sleep cycle disruptions is critical for long-term health. Poor sleep quality is linked to cardiovascular disease, diabetes, depression, weakened immune function, and cognitive decline. When left untreated, sleep disorders can worsen existing conditions and lead to new health concerns. Accurate diagnosis through sleep testing Sydney enables healthcare professionals to create targeted treatment plans that restore restorative sleep and support overall wellbeing.
How Should Patients Prepare for a Sleep Study?
Proper sleep study preparation begins 24 hours before your scheduled appointment. Avoid consuming caffeine in any form—coffee, tea, energy drinks, chocolate, or certain medications—as these substances can significantly alter your natural sleep patterns and compromise the accuracy of your test results. Alcohol should also be eliminated from your routine, as it affects sleep architecture and can mask or exaggerate certain sleep disorders.
Why is staying awake during the day so critical?
Resisting the urge to nap on your test day ensures you’ll be genuinely tired when it’s time for the study. Taking even a short nap can reduce your sleep drive, making it harder to fall asleep in an unfamiliar environment with sensors attached. This delay or difficulty sleeping can result in insufficient data collection, potentially requiring you to repeat the entire study.
What grooming steps should you follow?
Wash your hair thoroughly on the day of your sleep study, but skip all styling products. Hair gels, oils, sprays, conditioners, and leave-in treatments create a barrier between your scalp and the electrodes that measure brain activity. Clean, product-free hair allows sensors to make proper contact with your skin, ensuring clear signal transmission throughout the night.
How should you handle your medications?
Contact your healthcare provider well before your scheduled study to discuss medication adjustments. Some medications can interfere with sleep patterns or mask symptoms your doctor needs to observe. Your provider may ask you to:
- Temporarily discontinue certain sleep aids or sedatives
- Adjust the timing of medications that affect alertness
- Continue taking essential medications for chronic conditions
- Bring a complete list of all prescriptions, over-the-counter drugs, and supplements
What should you bring to the sleep center?
Pack comfortable, loose-fitting sleepwear that allows easy access for sensor placement. Bring your regular bedtime items like reading materials or a book, though electronic devices may be restricted. If you wear glasses or contact lenses, bring appropriate storage cases. Consider packing toiletries for your morning routine, as most sleep centers have shower facilities available after your study concludes.
Should you maintain your normal routine?
Stick to your typical daily schedule as much as possible. Eat regular meals at your
What Happens During a Sleep Study?
The Sleep Study Procedure
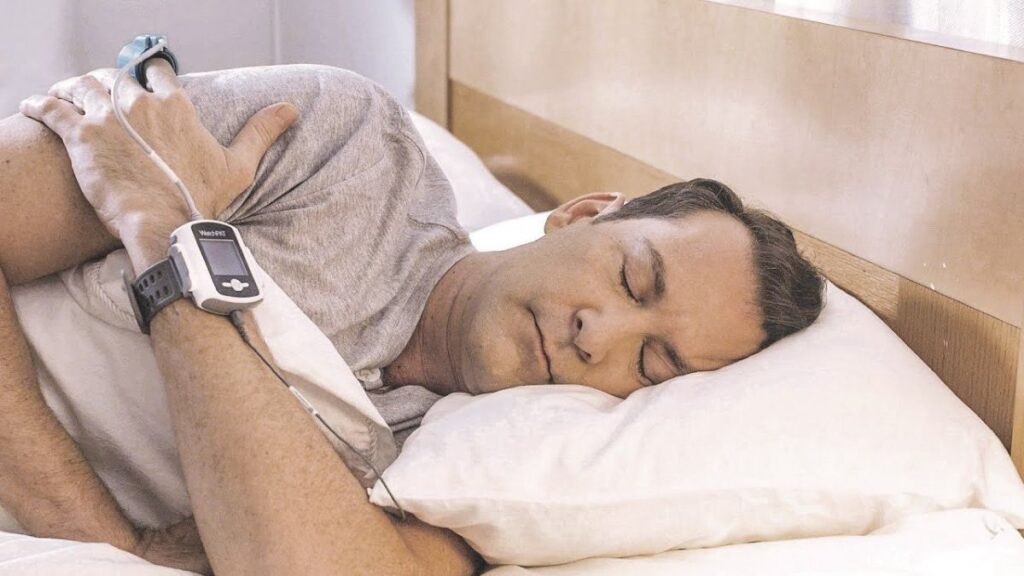
The sleep study procedure begins with a technologist carefully placing sensors on specific areas of your body using adhesive pads or medical tape. Electrodes are positioned on your scalp to record brain waves (EEG), on your chest to track heart rhythm (EKG), on your chin and legs to measure muscle tone (EMG), and near your eyes to detect eye movements (EOG). A pulse oximeter clips onto your finger to monitor oxygen levels throughout the night, while elastic belts wrap around your chest and abdomen to measure breathing effort.
Sensor attachment takes approximately 30 to 45 minutes to complete. The technologist ensures each electrode makes proper contact with your skin, sometimes using a gentle abrasive to improve signal quality. Wires from all sensors connect to a central recording device, though they’re arranged to allow natural movement during sleep. You can turn over, adjust your position, and sleep in your preferred posture without compromising data collection.
The Monitoring Environment
Sleep study rooms are designed to mirror comfortable hotel accommodations rather than clinical spaces. Each room typically features:
- A regular bed with quality linens and pillows
- Adjustable lighting and temperature controls
- A private bathroom
- Minimal medical equipment visible to reduce anxiety
- Dim lighting options for those who prefer not sleeping in complete darkness
Overnight Monitoring Process
Once sensors are in place and you’re settled in bed, overnight monitoring begins. A trained technologist observes your sleep from an adjacent control room using video feeds and real-time data from the sensors. They watch for technical issues like loose electrodes and can enter your room if adjustments are needed. Two-way audio systems allow you to communicate with staff throughout the night without getting out of bed.
The sensors work together to create a comprehensive picture of your sleep architecture. Brain wave patterns reveal which sleep stage you’re in at any moment, while respiratory sensors detect breathing pauses or shallow breathing. Heart rate monitors identify irregular rhythms that may correlate with breathing disruptions, and the pulse oximeter tracks how these events affect blood oxygen levels.
Most patients sleep for six to seven hours during the study, providing sufficient data for accurate analysis. The technologist continues recording until morning, capturing multiple complete sleep cycles that include both REM and non-REM
What Types of Sleep Tests Are Available?
There are three main types of sleep studies, each designed to evaluate different aspects of sleep disorders. The choice depends on your symptoms, suspected condition, and medical history.
1. Overnight Polysomnography
Overnight in-lab polysomnography is considered the gold standard among types of sleep studies. This comprehensive test takes place in a specialized sleep center where technologists monitor you throughout the entire night. The test captures detailed data across multiple body systems simultaneously:
- brain wave patterns
- heart rhythm
- breathing effort
- oxygen saturation
- muscle activity
- eye movements
- body position changes
In-lab testing provides the most complete picture of your sleep architecture. Technologists can observe you directly through video monitoring and respond immediately if sensors become dislodged or if you need assistance. This real-time supervision ensures high-quality data collection that might be compromised in an unsupervised setting.
The controlled environment allows for detection of complex sleep disorders beyond breathing problems. Conditions like REM sleep behavior disorder, periodic limb movement disorder, and unusual parasomnias require the extensive monitoring capabilities only available through full polysomnography.
2. Home Sleep Apnea Test
A home sleep apnea test offers a simplified alternative for patients with suspected obstructive sleep apnea. These portable devices focus primarily on respiratory measurements:
- airflow
- breathing effort through chest and abdominal belts
- oxygen levels via pulse oximetry
- sometimes heart rate and body position
Home testing provides convenience and lower cost compared to in-lab studies. You sleep in your own bed following your normal routine, which some patients find more comfortable than a clinical setting. The device arrives at your home with instructions for self-application, though some facilities offer brief training sessions.
This option works best for patients with clear symptoms of sleep apnea without complicating medical conditions. Home tests cannot diagnose sleep disorders unrelated to breathing, such as narcolepsy, restless legs syndrome, or insomnia. The limited sensor array means certain data points remain unmeasured.
3. Multiple Sleep Latency Test(MSLT)
The Multiple Sleep Latency Test serves a specialized purpose in evaluating excessive daytime sleepiness and narcolepsy. This daytime procedure follows an overnight sleep study and measures how quickly you fall asleep during scheduled nap opportunities
What Are the Risks or Discomforts Associated with Sleep Testing?
Sleep studies carry minimal medical risks and are considered safe diagnostic procedures. The most common issue patients encounter is mild sensor irritation from the adhesive pads that hold electrodes in place throughout the night.
The adhesive used to attach sensors may cause temporary redness or slight skin sensitivity, particularly for individuals with sensitive skin or allergies to certain adhesives. This irritation typically resolves within a few hours after sensor removal and rarely requires any treatment beyond basic skin care.
Physical discomfort represents another consideration, though it’s generally manageable. Patients often report an initial adjustment period as they become accustomed to:
- Multiple wires connected to various body parts
- Elastic belts positioned around the chest and abdomen
- A pulse oximeter clip attached to a finger
- Electrodes placed on the scalp, face, and legs
The sensation of being “tethered” to monitoring equipment can feel restrictive at first. Some patients find it challenging to move naturally or shift sleeping positions with sensors attached. The wires provide enough slack for normal movement, yet the awareness of being connected to equipment may prevent some individuals from achieving their typical sleep quality.
Sleeping in an unfamiliar environment adds another layer of discomfort. Despite sleep labs designing rooms to resemble comfortable hotel accommodations, many patients struggle to fall asleep as easily as they would at home. The knowledge that technologists are monitoring their sleep from another room, combined with the clinical setting, can create mild anxiety that affects sleep onset.
Claustrophobic feelings may arise if nasal cannulas or other breathing monitoring devices are required during the study. These devices rest near or in the nostrils to measure airflow, which some patients find bothersome or intrusive.
Sleep study risks remain exceptionally low compared to other medical procedures. No needles, medications, or invasive techniques are involved in standard polysomnography. The equipment simply records physiological data without altering body functions or introducing substances into the system.
Rare complications might include allergic reactions to electrode paste or adhesive materials, though sleep centers typically use hypoallergenic products to minimize this possibility. Patients with known skin sensitivities should inform technologists beforehand so alternative attachment methods can be arranged.
How Are Sleep Study Results Analyzed and Communicated?
Sleep study results analysis begins immediately after your test concludes, with trained sleep technologists reviewing the extensive data collected throughout the night. The typical turnaround time for complete results is approximately two weeks from your study date.
The Initial Technical Review
Sleep technologists serve as the first line of analysis, meticulously examining hours of recorded data from multiple monitoring systems. They score each epoch of sleep—typically divided into 30-second intervals—identifying sleep stages, respiratory events, limb movements, and cardiac irregularities. This detailed scoring process involves:
- Cataloging each instance of apnea or hypopnea
- Documenting oxygen desaturation events
- Recording arousals and awakenings
- Tracking body position changes
- Noting any unusual behaviors or movements
The technologist compiles these observations into a comprehensive data set, calculating critical metrics such as the Apnea-Hypopnea Index (AHI), oxygen nadir levels, and sleep efficiency percentages.
Board-Certified Sleep Specialist Interpretation
Once the technical scoring is complete, a board-certified sleep specialist review transforms raw data into actionable medical insights. These physicians—often certified in sleep medicine, pulmonology, or neurology—bring clinical expertise to the interpretation process. They correlate the quantitative measurements with your reported symptoms, medical history, and physical examination findings.
The specialist examines patterns that might indicate specific disorders. For instance, they differentiate between obstructive and central sleep apnea by analyzing chest and abdominal movement patterns alongside airflow measurements. They assess whether breathing disturbances occur predominantly during REM sleep or across all sleep stages, which influences treatment planning.
The Diagnostic Report
Your sleep specialist generates a detailed diagnostic report that includes:
- Summary of sleep architecture showing time spent in each sleep stage
- Respiratory disturbance index with severity classification
- Oxygen saturation data with lowest recorded levels
- Heart rate variability and rhythm abnormalities
- Limb movement analysis
- Formal diagnosis based on established clinical criteria
- Specific treatment recommendations tailored to your findings
Communication of Results
Most sleep centers schedule a follow-up appointment where your ordering physician or the sleep specialist discusses findings face-to-face.
What Information Do Sleep Study Results Provide?
Sleep study results deliver a comprehensive snapshot of your nighttime physiology, revealing patterns that explain daytime symptoms and sleep quality issues. The data captures everything from brain wave activity to oxygen levels, creating a detailed map of what happens while you’re unconscious.
Sleep Stages Data
Your report breaks down the time spent in each sleep phase throughout the night. Non-REM sleep divides into three stages: N1 (light sleep), N2 (intermediate sleep), and N3 (deep, restorative sleep). REM sleep, where most dreaming occurs, typically cycles every 90 minutes.
The results show whether you’re achieving adequate amounts of each stage. Healthy adults spend roughly 50% of sleep in N2, 20% in REM, 20% in N3, and 10% in N1. Deviations from these percentages can indicate specific disorders or explain why you wake feeling unrefreshed despite spending sufficient time in bed.
Sleep efficiency metrics reveal the percentage of time actually asleep versus lying awake. Numbers below 85% suggest difficulty initiating or maintaining sleep, pointing toward insomnia or other disruptions requiring intervention.
See Also : Understanding the sleep cycle
Breathing Irregularities Detection
The study quantifies respiratory events with precision. Apneas represent complete breathing pauses lasting 10 seconds or longer, while hypopneas indicate partial airflow reductions of 30% or more accompanied by oxygen drops or brief awakenings.
Your Apnea-Hypopnea Index (AHI) counts these events per hour of sleep:
- Normal: Fewer than 5 events per hour
- Mild sleep apnea: 5-14 events per hour
- Moderate sleep apnea: 15-29 events per hour
- Severe sleep apnea: 30 or more events per hour
Oxygen saturation measurements show how deeply these breathing disruptions affect your body. Normal levels hover around 95-100%, but repeated drops below 90% strain your cardiovascular system and fragment sleep architecture.
Cardiovascular Response Patterns
Heart rate data reveals how your cardiovascular system responds to sleep events. Apneas often trigger sudden heart rate increases
What Treatment Options May Follow Based on Sleep Testing Findings?
Positive airway pressure therapy stands as the primary treatment after sleep testing confirms obstructive sleep apnea. CPAP (continuous positive airway pressure) devices deliver a steady stream of pressurized air through a mask, keeping airways open throughout the night and preventing the repeated breathing interruptions that characterize this condition.
Your sleep specialist prescribes specific pressure settings based on data collected during your study. The recordings reveal exactly when and how often your airway collapses, allowing clinicians to determine the minimum pressure needed to maintain open airways without causing unnecessary discomfort.
Customizing PAP Therapy Settings
Device calibration depends on several factors identified in your sleep study results:
- Apnea-Hypopnea Index (AHI) severity determines baseline pressure requirements
- Oxygen desaturation patterns indicate how aggressively treatment needs to address breathing disruptions
- Sleep position data shows whether pressure adjustments are needed for different sleeping postures
- Mask leak measurements help identify the most suitable mask style for your facial structure
Some patients receive prescriptions for BiPAP (bilevel positive airway pressure) instead of CPAP. This variation provides two pressure levels—higher during inhalation and lower during exhalation—making breathing feel more natural for individuals who struggle with constant pressure or have certain respiratory conditions.
Alternative Treatments Beyond PAP Devices
Sleep testing findings may point toward other therapeutic approaches depending on your specific diagnosis:
Oral appliances work for mild to moderate sleep apnea by repositioning the jaw and tongue to prevent airway collapse. Your study results help determine whether this option suits your particular breathing pattern and anatomical factors.
Positional therapy becomes relevant when test data shows apneas occur primarily while sleeping on your back. Simple devices or specialized pillows encourage side-sleeping positions that naturally reduce airway obstruction.
Lifestyle modifications receive targeted recommendations based on study observations. Weight loss plans, sleep schedule adjustments, or alcohol reduction strategies address contributing factors identified during monitoring.
Treatment for Other Sleep Disorders
Narcolepsy diagnosed through MSLT testing typically requires stimulant medications to manage excessive daytime sleepiness. Your test results showing how quickly you enter REM sleep can guide medication selection and dosing strategies.
What Should Patients Expect After Completing a Sleep Study?
Sensor Removal Process
The sensor removal process takes only a few minutes and is handled entirely by trained sleep center staff. Technologists carefully remove each electrode and sensor from your skin, scalp, chest, and limbs using gentle techniques that minimize any discomfort. The adhesive used to attach sensors typically comes off easily, though you may notice some residue on your skin or hair that can be washed away with normal bathing.

Post-Sleep Study Expectations
Post-sleep study expectations include immediate freedom to resume your regular daily activities. You can drive yourself home, go to work, or continue with any plans you had scheduled for that day. No recovery period is necessary since sleep testing is completely non-invasive and doesn’t involve medications or procedures that would impair your functioning.
Some patients notice slight redness or minor irritation where sensors were attached, particularly on sensitive skin areas. These effects typically disappear within hours and rarely require any treatment. If you had electrodes placed on your scalp, your hair may feel slightly sticky or tangled from the conductive paste used, but a regular shower resolves this completely.
The sleep center staff will provide information about when to expect your results, usually within two weeks. They’ll explain the next steps in the process, including how your healthcare provider will contact you to discuss findings and any recommended treatments. You don’t need to follow any special instructions or restrictions after leaving the facility.
Most patients report feeling tired after a sleep study since sleeping in an unfamiliar environment with sensors attached often results in less restful sleep than usual. This fatigue is normal and temporary. Taking it easy for the remainder of the day can help, though it’s not medically necessary. Your natural sleep patterns will return to normal that same night when you sleep in your own bed without monitoring equipment.
Conclusion
Understanding the importance of knowing about sleep testing empowers you to approach the process with confidence rather than anxiety. Sleep studies are straightforward, non-invasive procedures designed to improve your quality of life by identifying treatable conditions that may be disrupting your rest.
Everything You Need to Know Before Getting Sleep Testing comes down to preparation, understanding the process, and maintaining open communication with your medical team. Ask questions about sensor placement, what the technologists will be monitoring, and how long results typically take. Your healthcare provider can explain why they’ve recommended testing and what specific concerns they hope to address.
Sleep disorders affect millions of people, yet many remain undiagnosed simply because patients hesitate to seek evaluation. The testing process itself poses minimal risk while offering substantial benefits through accurate diagnosis and targeted treatment plans. Whether you undergo an in-lab polysomnography or a home sleep test, the data collected provides invaluable insights into your sleep health.
However, neglecting sleep issues can have severe consequences. The health effects of sleep deprivation can be profound, impacting everything from physical well-being to mental clarity and daily functioning. Don’t let uncertainty prevent you from taking this important step toward better sleep. Discuss any concerns about the procedure, costs, or potential findings with your doctor beforehand. The more informed you feel going into your sleep study, the more relaxed you’ll be during the actual test—which can lead to more accurate results.
Taking action through sleep testing demonstrates a commitment to addressing problems rather than simply living with fatigue, snoring, or other symptoms. The path to restorative sleep often begins with a single night of monitored rest.
Related : Get a Better Night’s Rest with a Sleep Study Canberra




